FREE ACCESS: Jamaica Lagging Behind International Standard for Reporting Post-Vaccine Deaths
Part 2
18º North promised to make this series on vaccine safety surveillance available for free after making it available to paid subscribers.
You can help 18º North do more original, in-depth reporting by taking out a paid subscription. The cost is US$11.50 a month or US$115 a year with sales tax included.
Jamaica is lagging in its effort to conform to the internationally-approved protocol of reporting all adverse responses post-vaccination, including deaths.
Not only is its Ministry of Health & Wellness unaware of some of the deaths that are occurring post-vaccination - potentially compromising its ability to conduct effective safety surveillance - but even when it knows about some of the deaths, it has failed to communicate them in a timely and transparent way to the public.
For years, the Pan American Health Organization, the Regional Office for The Americas of the World Health Organization (WHO), has recommended that all countries keep track of side effects or adverse events following immunization (AEFI). AEFI is defined as “any untoward medical occurrence that follows immunization and that does not necessarily have a causal relationship with the usage of the vaccine.”
In December, the WHO also released a Safety Surveillance Manual on Covid-19 vaccines, which stated, “Timely detection and reporting of adverse events following COVID-19 immunization is the first step in the continuous verification of vaccine safety... including incidents of substandard or counterfeit vaccines.”
On communication with the public, it advised, “Be open and transparent about vaccine safety by providing access to all information, not withholding any, even when the facts are yet to be fully established. There is no evidence to support the assumption that the public will panic if they have access to accurate information in a crisis. Lack of honesty and withholding information can erode trust.”
It said, “Communication that is transparent, timely, empathic and acknowledges uncertainty can help boost people’s trust in health authorities, which in turn can positively influence people’s willingness to be vaccinated.”
How Jamaica Changed Its Reporting on Adverse Events Following Immunization
Jamaica’s Ministry of Health & Wellness initially heeded this advice, when about a month into its vaccination program - on April 14 - it presented a summary of 76 events supposedly attributable to vaccination or immunization (ESAVI).
At the time, five were said to have been serious, with patients experiencing either severe muscle pain or anaphylactic reactions, which are potentially life-threatening allergic responses. One of the five was a death, which was said, at the time, to have been under investigation.
The Chief Medical Officer Dr. Jacquiline Bisasor-Mckenzie, who is responsible for ensuring that the health status of the Jamaican people achieves a high standard and conforms to international and national development goals, made a commitment to the public then, “We will be transparent in our reporting.”
“All the reports that come in we will report them, and so if we have persons that would have died after getting the vaccine, then we will report it. If we’ve had persons experiencing severe problems after the vaccine, then we will report it,” she said without giving a timeline for these reports.
“This is how we analyze information. We look at patterns right across the world because these reports are submitted to the global committee that monitors these to see if there’s any kind of relationship.” (The global database to which this information is submitted is called VigiBase. There’s also VigiCarib that pulls data from VigiBase for the Caribbean region.)
Video: On April 14, Chief Medical Officer Dr. Jacquiline Bisasor-Mckenzie promised transparent reporting on adverse events after vaccine but did not give a timeline for the frequency of the updates. Credit: MOH
But when 18º North asked for an update a month later at a May 13 press conference regarding how many deaths there had been after vaccination, regardless of cause, the ministry appeared less willing to immediately share the information.
“We are doing a complete investigation looking at all aspects of the history of persons who may have died after being vaccinated in order to ascertain cause and effect,” said Dr. Melody Ennis, who is overseeing the country’s vaccination program. “As soon as we complete the investigation, we will share the details.”

More than three months later and an 18º North investigation showing there have been at least eight deaths post-vaccination regardless of cause, there has still been no further presentation to the Jamaican public about adverse events. Meanwhile, similar reports from some of the country’s key international partners - like the United States, United Kingdom and Canada - are published weekly in their own countries.
*In its Global Manual on Surveillance of Adverse Events Following Immunization, the WHO advises countries that when communicating with the media, “waiting for the conclusion of an investigation is rarely possible.”
“Information may need to be disseminated early and often, and it is vital to be honest about what is known and what is not known, and to avoid being evasive and unresponsive.”
Dr. Susan Lowe, an integrative general practitioner in Jamaica that employs a mix of natural therapies and traditional Western medicines, like antibiotics and vaccines, to treat patients, says the change by the ministry from announcing deaths under investigation to investigating first before sharing the information “could be a genuine scientific move” in stating how something occurred. On the other hand, it could also be “fear that the anti-vaxxers will jump and say ‘the vaccine is causing deaths.’ ” In Jamaica, vaccine hesitancy is already one of the highest in the world, with less than a third of persons saying they would take a Covid-19 vaccine if it was offered to them for free, according to a Gallup poll conducted last year.
But regardless of the reason, Dr. Kevin Harvey, Head of School of Public Health & Health Technology at the University of Technology (UTech) in Jamaica believes that the ministry should be more forthcoming about post-vaccine deaths and report them in the same way that Covid-19 deaths are reported, which often include deaths under investigation.
“Giving as much information as you can is really the best way to go,” he said. “If the public perceives that the government or the ministry is hiding something, then it could also lead to further mistrust.”
The United States VAERS System
Balancing the desire for transparency against the possibility of misuse of the information can be tricky.
On the one hand, a problem becoming public might encourage others with similar experiences to come forward so it can be studied against the typical rates of illness that existed before vaccination and a determination made about whether a safety signal needs to be flagged or whether there is some kind of immunization error.
On the other hand, there are some persons who will use the information to quickly conclude the vaccine is causing deaths even if the science shows otherwise. This could have damaging consequences for immunization coverage and incidence of disease.
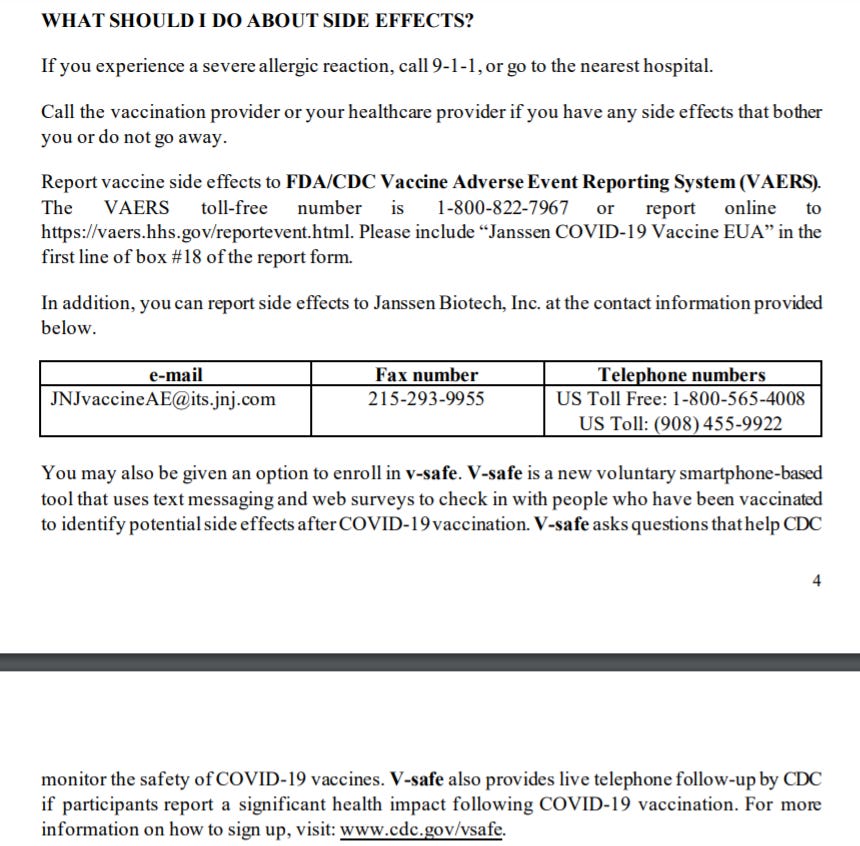
In the U.S., the Vaccine Adverse Event Reporting System, VAERS, run by the Food & Drug Administration (FDA) and the Centers for Disease Control and Prevention (CDC) is public, and anyone can file a report.
However, reporting into VAERS is voluntary, except for healthcare providers who are required by law to report all deaths and serious events after vaccination regardless of cause.
The CDC has acknowledged that relying on the public to report adverse events has led to significant underreporting over the years. When the Covid-19 vaccines were rolled out, it added a system called v-safe, where recipients who choose to enroll in the program receive regular text messages to complete short online health surveys for up to a year. Those who indicate seeking medical care are contacted by v-safe’s call center and encouraged to complete a VAERS report.
VAERS has been credited for spotting various side effects, including, more recently, the rare and serious occurrence of thrombosis with thrombocytopenia syndrome (TTS) or blood clots with low platelet counts following the Johnson & Johnson/Janssen Covid-19 shot. Though only six individuals were reported to have experienced the condition out of more than 6.8 million doses administered, on April 13, the FDA and CDC announced a pause to explore a possible link. Nine more cases were confirmed, and the exploration eventually revealed a plausible causal relationship with the J&J shot.
The CDC and FDA subsequently recommended restarting use of the vaccine on April 23 with an advisory to be included about the risk, concluding that the incidence of the condition was rare and that the benefits of the vaccine outweighed the risk.
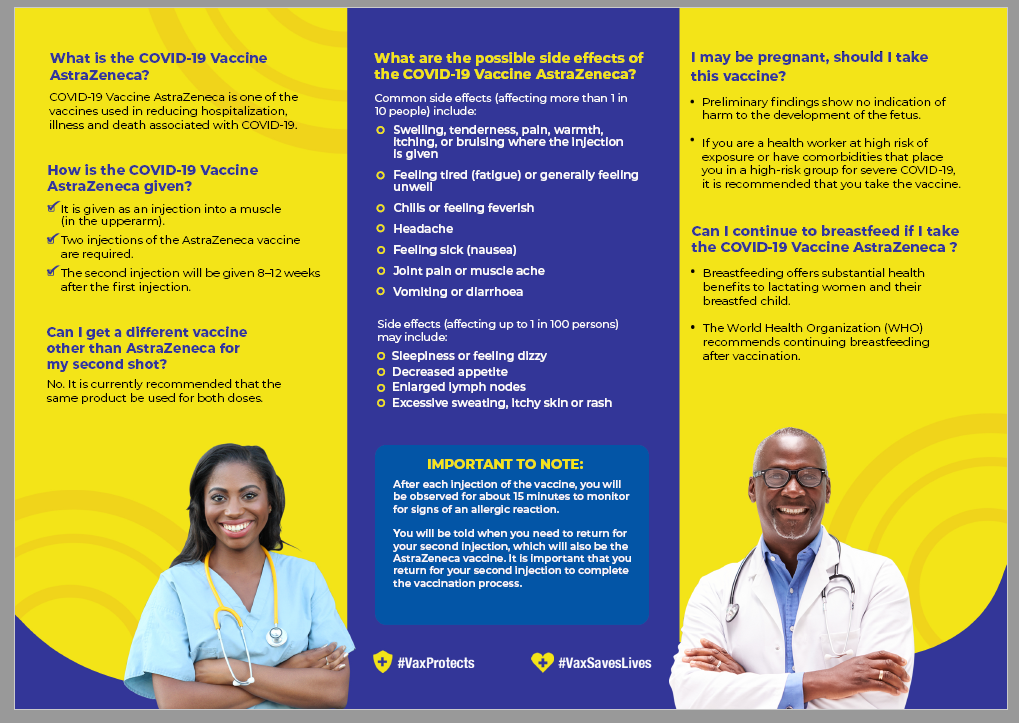
A similar conclusion was reached by the WHO, which reported that TTS was also plausibly linked to the J&J and AstraZeneca vaccines. AstraZeneca has been the main brand being administered by the Jamaican government, although it just recently got a small donation of J&J shots.
Being Transparent Carries Risk of Misinformation
The downside of VAERS is that it has been used for misinformation campaigns as well.
Data from VAERS have been unscientifically cited on social media as evidence that Covid-19 vaccines are causing thousands of deaths.
There was even a "completely made-up" report that spread on social media of a two-year-old girl who died in the state of Virginia less than a week after receiving a shot during vaccine experiments on children. A professional athlete was listed as the patient and a world leader's name used for the person who reported the incident. The report was eventually removed from VAERS.
Still, even with this kind of misuse of the system and misrepresentation of the data, scientists in the U.S. still maintain VAERS should remain open to the public.
“Transparency is preferred,” explained Laura Scherer, Assistant Professor at the University of Colorado School of Medicine who has studied health misinformation online. “But this transparency also comes with a responsibility and burden, put mainly on scientists and the media, to continue to teach the public about the limitations of these data.”
On its website, the CDC lays out that as of July 26, more than 342 million doses of Covid-19 vaccines were administered in the U.S. with VAERS receiving 6,340 reports of death (0.0019%) among people who were vaccinated.
It continues, “A review of available clinical information, including death certificates, autopsy, and medical records, has not established a causal link to COVID-19 vaccines. However, recent reports indicate a plausible causal relationship between the J&J/Janssen COVID-19 Vaccine and TTS, a rare and serious adverse event—blood clots with low platelets—which has caused deaths.”
There were three such deaths out of almost eight million J&J doses administered in the U.S. at the time, according to a CDC release on May 7. The CDC told 18º North on July 8 that it’s still reporting three deaths despite an increase in the administration of J&J shots to about 13 million displayed elsewhere on its website. (In the U.K., there have been 71 such deaths after 47.5 million doses of the AstraZeneca vaccine as of July 14, according to its Yellow Card report on adverse events.)
AstraZeneca and J&J did not reply to requests for comment.
How Jamaica Monitors and Reports on Vaccine Safety
In Jamaica, the standard protocol is that after vaccination, persons are observed for 10 to 30 minutes to see if there are any adverse reactions.
Anything after that, persons are advised on the information brochure to “seek medical attention” or report side effects to a doctor, nurse or local health department.
But unlike the information brochures in the U.S. that clearly state how to file an adverse report, the Jamaican version has no mention of the ESAVI form on the ministry’s website that’s used to report adverse concerns. When 18º North visited a recent vaccination blitz for administering second doses, there was no public education about it either.
Most of the several health aides polled by 18º North that day said they hadn’t heard about the form, and agents who answered the Covid-19 vaccine information line also were not aware of it when 18º North called on two separate occasions. However, several doctors told 18º North that the health ministry had sensitized them about the form and how to report on adverse concerns.

When 18º North asked Dr. Ennis why regular members of the public aren’t made aware of the form at vaccination since they can also file a report, she merely emailed that the form is publicly available.
She continued, “Persons are advised and encouraged to report adverse events using which ever platform the find comfortable. However, we do prefer if it is reported into a healthcare provider who can make an assessment, allay fear or initiate treatment if necessary.”
But even the healthcare providers themselves don’t seem fully clear on what and when to report.
Though Dr. Ennis maintains that adverse events should be reported within the first year after vaccination regardless of suspicion of cause from the vaccine, three different Jamaican doctors with whom 18º North interacted over the last three months were quick to determine that two hospitalizations and three deaths were not adverse events because they believed they weren’t caused by the vaccine, and so some of the cases were not reported for analysis at the national level.
The doctors are also under the impression that reporting is voluntary in Jamaica, and Dr. Ennis, who is running the overall vaccination program, told 18º North that she too was unclear about whether there is a legal requirement to report.
But 18º North came across Regulation 70 of The Food & Drugs Act of 1975 on the Ministry of Health’s website that states, “Where any person receives any report of any unexpected side effects, injury, toxicity or sensitivity reaction associated with clinical uses, studies, investigation and tests respecting any new drug, he shall immediately inform the Minister thereof, furnishing him with the full information available.”
Regulation 87 of the Act also states, “Any person who fails to comply with any of these Regulations shall be guilty of an offence, and upon summary conviction before a Resident Magistrate shall be liable to a fine not exceeding two thousand dollars [US$13] or to a term of imprisonment not exceeding twelve months.”
Jamaican attorney Michelle Thomas, who has researched public health vaccination laws across the Caribbean for PAHO, believes that based on this law, the health ministry has a duty to educate the public, not just doctors, on how to go about reporting adverse events.
“Just as how they’re saying ‘wear a mask, social distance’, they also need to say ‘if you take a vaccine and have a side effect, you must report this’,” she said. “Once we have this information provided we can create a range of side effects, so when a person wants to decide whether to take the vaccine, they can do so from an informed standpoint.”
Dr. Harvey, head of the School of Public Health at UTech, further suggests the health ministry create a more formal structure for doctors to report adverse events post-vaccination in the same way, for example, that they’ve been required to report a Class 1 Notifiable disease like malaria or meningitis within 24 hours based on the mere suspicion of disease.
However, this suggestion was dismissed by Dr. Ennis who said, “It has no application to that.”
“If all our colleagues need further guidance, then they need to speak to their regional technical directors, they need to speak to the ministry, so that they can be clear. This is not something to be discussed in the press,” she said. “It’s something clinical.”
In its Global Manual on Surveillance on Adverse Events Following Immunization, the WHO identified several reasons why immunization service providers may not report AEFIs. These include: considering that the event did not occur after immunization; lack of knowledge about the reporting system and process; apathy, procrastination, lack of interest or time, and inability to find the reporting form; fear that the report will lead to personal consequences; guilt about having caused harm and being held responsible for the event; and diffidence (shyness) about reporting an event when not confident about the diagnosis.
To combat this problem, it suggests, “Staff must be encouraged to report adverse events without fear of penalty. The aim is to improve systems or provide further training, and not to blame individuals.”
Editor’s Notes:
*In PAHO’s Guide for the Preparation of a Risk Communication Strategy for COVID-19 Vaccines, there is some guidance that seems to conflict with that of the WHO although it wasn’t specifically addressing AEFI. It states, “Confirm all information before issuing it. Do not talk about assumptions or preliminary information. Relative information leads to discursive confusion.” However, in another PAHO document, Crisis Communication Related to Vaccine Safety: Technical Guidance, on how to communicate with the public in a particular hypothetical scenario where there is a child’s death after vaccine, it goes along with WHO guidance and states, “communicate about the event and the preliminary findings of the investigation as soon as possible.”
18º North asked for clarity from PAHO, but it did not respond in time for publication.
**Story has been updated from its original version.
To be continued:
NEXT: As more persons report alleged injuries from vaccines, how will Jamaica handle possible liabilities?
If you think this kind of reporting is important, help us do more. Become a paid subscriber today:
Related Stories:
Jamaican Doctor Hospitalized Following Second Dose of Covid-19 Vaccine; Flown to U.S. for Treatment